Weight Loss Drugs (GLP-1) Coverage
GLP-1 medications, also known as glucagon-like peptide-1 receptor agonists (GLP-1Ras), mimic the hormone GLP-1 in the body. This hormone helps control blood glucose levels, insulin production, and feelings of fullness. GLP-1 medications treat type 2 diabetes and assist in weight management.
The guidelines for weight loss drugs are continually being updated.Aetna/Aetna Funding Advantage
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Yes
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- GLP-1 Coverage Details and Criteria:
- Clinical criteria can be found on the Aetna public site for providers, health care professionals also may obtain information by calling the Pharmacy Management Precertification Unit at 1-800-414-2386, or they can register to use the password-protected provider website. Visit www.aetna.com, select "Doctors & Hospitals" and choose "Physician Self-Service." Once registration is completed, healthcare professionals may use our online Precertification/medical exception email request form.
- Clinical Policy Bulletins on the public provider site here, can be shared with members/providers for criteria. The bottom of the page has a “Pharmacy Criteria” search box.
- GLP-1 Coverage Details and Criteria:
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- Because coverage approval can vary depending on the member's plan, please direct members to the CPB link and their specific plan benefits to check if coverage is approved. The Clinical Policy Bulletins available on the public provider site can be shared with members and providers for reference on eligibility criteria. At the bottom of the page, there is a “Pharmacy Criteria” search box that can be utilized.
- Is the coverage full or is it at 50%?
- Because coverage approval can vary depending on the member's plan, please direct members to the CPB link and their specific plan benefits to check if coverage is approved. The Clinical Policy Bulletins available on the public provider site can be shared with members and providers for reference on eligibility criteria. At the bottom of the page, there is a “Pharmacy Criteria” search box that can be utilized
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Because coverage approval can vary depending on the member's plan, please direct members to the CPB link and their specific plan benefits to check if coverage is approved. The Clinical Policy Bulletins available on the public provider site can be shared with members and providers for reference on eligibility criteria. At the bottom of the page, there is a “Pharmacy Criteria” search box that can be utilized.
- Supporting Collateral:
- Middle Market Formulary: The formularies indicate which brands are covered, the pharmacy tier, and if step therapy/prior authorization is required. Find a Medication: Prescription Drug List (Formulary), Coverage & Costs | Aetna
- Middle Market (Fully Insured) – Advanced Control Plan – California
- Middle Market and Small Group (AFA) - Advanced Control Plan
- Small Group Formulary:
- For the AFA small group level-funded plans, coverage for weight loss medications is excluded.
- On the CA ACA plans the following applies:
- There are two separate formularies, one for HMO and one for PPO.
- 2025 Formulary links:
- Middle Market Formulary: The formularies indicate which brands are covered, the pharmacy tier, and if step therapy/prior authorization is required. Find a Medication: Prescription Drug List (Formulary), Coverage & Costs | Aetna
- Covered Medications:
- Here are the 2025 ACA PPO formulary medications for this class (found HERE):

- The HMO formulary includes the following:
- Trulicity – Tier 2 (page 79), ST/Ql
- Victoza – Tier 3 (page 79), ST/Ql
- Xultophy - Tier 3 (page 80), ST
- Here are the 2025 ACA PPO formulary medications for this class (found HERE):
Anthem Blue Cross (CA)
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Yes
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- Yes.
When prescribed solely to lose weight, except for the Medically Necessary treatment of morbid obesity. Members who are prescribed weight loss drugs that are Medically Necessary for the treatment of morbid obesity may be required to enroll in a comprehensive weight loss program, which is approved and covered by the Plan, for a reasonable period before or concurrent with receiving the Prescription Drug.
- Yes.
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- Yes.
Members who are prescribed weight loss drugs that are Medically Necessary for the treatment of morbid obesity may be required to enroll in a comprehensive weight loss program, which is approved and covered by the Plan, for a reasonable period before or concurrent with receiving the Prescription Drug.
- Yes.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Yes.
Members who are prescribed weight loss drugs that are Medically Necessary for the treatment of morbid obesity may be required to enroll in a comprehensive weight loss program, which is approved and covered by the Plan.
- Yes.
- Supporting Collateral:
- Covered Medications:
- Ozempic, Trulicity, and Victoza - tier 2 but needs prior authorization.
- Trulicity and Bydureon - non-formulary. Needs prior authorization.
- Mounjaro is non-formulary/specialty- it needs prior authorization.
- Wegovy is non-formulary; it will need prior authorization. This drug was recently approved for Cardiovascular risk reduction.
- Zepbound is non-formulary and will require PA. This is the drug that might be the hardest to approve since it is only approved for weight loss.
Anthem Blue Cross Blue Shield (NV)
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Yes
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- Click HERE to access Approval Criteria (page 2).
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- Prior authorization – 1 year.
- Is the coverage full or is it at 50%?
- Click HERE to access Approval Criteria (page 2).
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Click HERE to access Approval Criteria (page 2).
- Supporting Collateral:
- Click HERE to view the GLP-1 Receptor Agonists and GIP-GLP-1 Receptor Agonists NTL list.
- Covered Medications:
- Glucogon-Like-Peptide-1 (GLP-1) Receptor Agonists:
- Ozempic (semaglutide)
- Rybelsus (semaglutide)
- Trulicity (dulaglutide)
- Victoza (liraglutide)
- Adlyxin (lixisenatide)
- Bydureon (exenatide extended release) Bydureon BCise (exenatide extended release)
- Byetta (exenatide)
- Glucose-Dependent Insulinotropic Polypeptide (GIP)/Glucogon-Like-Peptide-1 (GLP-1) Receptor Agonists:
- Mounjaro (tirzepatide)
- Glucogon-Like-Peptide-1 (GLP-1) Receptor Agonists:
CalCPA
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Yes, all CalCPA Health plans cover GLP-1 for weight loss as medically necessary. through their Self-Injectable benefit on their Prescription Drug Plan.
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- BMI greater than or equal to 32 or greater than or equal to 27 with documentation of two comorbid conditions before starting treatment.
- Must enroll in the EncircleRx Omada virtual health program which will require 4 weigh ins and 4 interactions on the Omada app.
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- N/A.
- Is the coverage full or is it at 50%?
- Refer to the Self-Injectable benefits on the Prescription Drug Plan.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Yes, they must enroll and stay active in the Omada virtual health program.
- Supporting Collateral:
- Covered Medications:
- Dulaglutide: Brand name Trulicity
- Tirzepatide: Brand names Mounjaro and Zepbound
- Semaglutide: Brand names Ozempic, Wegovy, and Rybelsus
- Lixisenatide: Brand Name Adlyxin
- Liraglutide: Brand names Victoza and Saxenda
- Exenatide: Brand names Byetta and Bydureon
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- CCHP does not cover any drugs solely for weight loss.
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- N/A.
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- N/A.
- Is the coverage full or is it at 50%?
- N/A.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- N/A.
- Supporting Collateral:
- N/A.
- Covered Medications:
- Dulaglutide: Brand name Trulicity
- Trulicity for Diabetes type 2 is covered as of 1/15/2025 (subject to change).
- Exenatide: Brand names Byetta and Bydureon
- Byetta and Bydureon for Diabetes type 2 is covered as of 1/15/2025 (subject to change).
- Liraglutide: Brand names Victoza and Saxenda
- Liraglutide for Diabetes type 2 is covered as of 1/15/2025 (subject to change).
- Lixisenatide: Brand Name Adlyxin
- Not covered.
- Semaglutide: Brand names Ozempic, Wegovy, and Rybelsus
- Ozempic and Rybelsus for Diabetes type 2 is covered as of 1/15/2025 (subject to change).
- Wegovy for cardiovascular risk reduction only is covered as of 1/15/2025 -needs PA/criteria to be met (subject to change).
- Tirzepatide: Brand names Mounjaro and Zepbound
- Mounjaro for Diabetes type 2 is covered as of 1/15/2025 (subject to change).
- Dulaglutide: Brand name Trulicity
Cigna
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Yes.
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- Only fully insured HMO plans allow a medical necessity override for weight loss drugs. This override requires a diagnosis of morbid obesity and approval from the provider. Otherwise, GLP-1 medications are covered solely for diabetes management and weight control. All plans include coverage for diabetes-related GLP-1s.
- For OAP plans under Level Funded plans, clients have the option to elect coverage for these weight loss drugs, which typically results in a pricing increase of 2.5-3%.
- If this optional coverage is chosen, prior authorization is required to ensure that the medications are prescribed according to FDA guidelines. Once approved, these medications will be covered under Cigna’s formulary, and the specific coverage details will depend on the drug in question if the weight loss rider is purchased.
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- Pending
- Is the coverage full or is it at 50%?
- Pending
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Pending
- Supporting Collateral:
- Click HERE for more details about the buy-up rider.
Log in to the myCigna® App or myCigna.com® to use the Price a Medication tool to see how much your medication costs. - Your Guide to EncircleRx for Cigna Healthcare: Tackling the GLP-1 trend
- Click HERE for more details about the buy-up rider.
- Covered Medications:
- These medications may need approval from Cigna Healthcare before the plan will cover them. They may also have quantity limits.
- Adipex-P®
- benzphetamine
- Contrave®
- diethylpropion/diethylpropion ER
- ImcivreeTM 4
- LomairaTM
- Orlistat
- phendimetrazine/phendimetrazine ER
- phentermine
- Qsymia®
- Saxenda®
- Wegovy®
- Xenical®
- ZepboundTM
- These medications may need approval from Cigna Healthcare before the plan will cover them. They may also have quantity limits.
Health Net
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
-
Yes. All weight loss drugs require prior approval based on Health Net’s drug use guidelines
-
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- For approval, Health Net Medical Necessity criteria must be met based on:
- BMI (Body Mass Index)
- Documentation of member’s baseline and current height and body weight within the last 30 days
- Other medical issues
- Documentation supporting member’s participation in a Health Net-approved weight loss program (e.g., Weight Watchers) or other weight loss programs recommended by the prescriber that involves:
- a reduced calorie diet
- increased physical activity and
- behavioral modification.
- For approval, Health Net Medical Necessity criteria must be met based on:
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- No, however, Health Net will requalify.
- Is the coverage full or is it at 50%?
- Benefits will depend on the plan enrolled on.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Yes, documentation supporting member’s participation in a Health Net-approved weight loss program (e.g., Weight Watchers) or other weight loss programs recommended by the prescriber that involves:
- a reduced calorie diet
- increased physical activity and behavioral modification.
- Yes, documentation supporting member’s participation in a Health Net-approved weight loss program (e.g., Weight Watchers) or other weight loss programs recommended by the prescriber that involves:
- Supporting Collateral:
- To request prior authorization, the prescriber must complete and fax a Prior Authorization form (PDF) to 866-399-0929.
- To access Pharmacy Prior Authorization Guidelines, please refer to:
Health Net Commercial Drug Coverage Policies | Health Net - To access the List of Covered Drugs based on your group size, please refer to:
Employer Group Drug List | Health Net
- Covered Medications:
-
Drug Name FDA Approved Indications Notes Ozempic Self-injection
Dosing once a weekOZEMPIC® is a glucagon-like peptide 1 (GLP-1) receptor agonist indicated as: • an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.
• to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes mellitus and established cardiovascular disease.Weight Loss – Not Covered
Coverage Requires prior authorization. Based on BMI and other medical conditionsSaxenda (self-injected medication) Dosing is daily SAXENDA® is a glucagon−like peptide−1 (GLP−1) receptor agonist indicated:
• as an adjunct to a reduced calorie diet and increased physical activity for chronic weight management.
• to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes mellitus and established cardiovascular disease.
Requires 6 months participation in a lifestyle modification / weight loss program that includes a lifestyle program, a reduced calorie diet and increased physical activity before requesting prior authorization.- Adult patients with an initial body mass index (BMI) of:
- 30 Kg/m2 or greater or
- 27Kg/m2 or greater in the presence of at least one weight-related medical condition (e.g., hypertension, type 2 diabetes mellitus, dyslipidemia
Weight Loss – is Covered
Coverage Requires prior authorization. Based on BMI and other medical conditionsWegovy
(self-injected medication) Dosing is weeklyWEGOVY® is a glucagon-like peptide-1 (GLP-1) receptor agonist indicated in combination with a reduced calorie diet and increased physical activity:
• to reduce the risk of major adverse cardiovascular events (cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke) in adults with established cardiovascular disease and either obesity or overweight.
• to reduce excess body weight and maintain weight reduction long term in: • Adults and pediatric patients aged 12 years and older with obesity
• Adults with overweight in the presence of at least one weight-related comorbid condition. Requires 6 months participation in a lifestyle modification /weight loss program that includes a lifestyle changes, a reduced calorie diet and increased physical activity before requesting prior authorization.- Adult patients with an initial body mass index (BMI) of:
- 30 Kg/m2 or greater or
- 27Kg/m2 or greater in the presence of at least one weight-related medical condition (e.g., hypertension, type 2 diabetes mellitus, dyslipidemia
Weight loss is covered. Coverage Requires prior authorization. Based on BMI and other medical conditions. Zepbound (self-injected medication) Dosing is weekly ZEPBOUND® is a glucose-dependent insulinotropic polypeptide (GIP) receptor and glucagon-like peptide-1 (GLP-1) receptor agonist indicated in combination with a reduced-calorie diet and increased physical activity: - to reduce excess body weight and maintain weight reduction long term in adults with obesity or adults with overweight in the presence of at least one weight-related comorbid condition.
- to treat moderate to severe obstructive sleep apnea (OSA) in adults with obesity.
- Adult patients with an initial body mass index (BMI) of:
- 30 Kg/m2 or greater or
- 27Kg/m2 or greater in the presence of at least one weight-related medical condition (e.g., hypertension, type 2 diabetes mellitus, dyslipidemia
Weight loss is covered. Coverage Requires prior authorization. Based on BMI and other medical conditions Mounjaro
Dosing is weeklyMOUNJARO® is a glucose-dependent insulinotropic polypeptide (GIP) receptor and glucagon-like peptide-1 (GLP-1) receptor agonist indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus Weight loss is not covered - Adult patients with an initial body mass index (BMI) of:
-
Hometown Health
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- No, Hometown Health only covers these drugs with qualifying Diabetes diagnosis codes, not for weight loss.
The coverage varies by plan, tier, and drug.
- No, Hometown Health only covers these drugs with qualifying Diabetes diagnosis codes, not for weight loss.
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- N/A.
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- N/A.
- Is the coverage full or is it at 50%?
- N/A.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- N/A.
- Supporting Collateral:
- N/A.
- Covered Medications:
- N/A.
MediExcel Health Plan
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- No.
MediExcel providers adhere to medical practice standards in Mexico which do not approve the use of GLP-1 medications for weight loss purposes. Furthermore, MediExcel Health Plan does not cover these medications for weight loss nor glucose management.
- No.
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- Excel Hospital/MediExcel Medical Group Mexicali offers a weight loss program consisting of internal medicine, nutrition, and psychology office visits. However, none of these options involve the use of GLP-1 medications.
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- N/A.
- Is the coverage full or is it at 50%?
- N/A.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- MediExcel Health Plan offers a weight loss program for members, where they may qualify for bariatric surgery after losing 10% of their initial body weight. However, this program does not qualify for, nor does it cover weight loss medications.
- Supporting Collateral:
- Please reference the bariatric surgery policy covered in pages 3 and 4 of this document.
- Covered Medications:
- MediExcel providers adhere to Mexico’s medical practice standards for weight loss; the medications listed above are only approved by COFEPRIS (primary regulatory authority for health in Mexico) for glucose management. However, MediExcel Health Plan does not cover these GLP-1 medications for weight loss nor glucose management.
Nippon Life Benefits
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Weight loss drug coverage can vary by plan and state requirements.
If a plan allows for weight loss drugs, coverage is subject to medical necessity which includes a Prior Authorization review.
- Weight loss drug coverage can vary by plan and state requirements.
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- Prior authorization may require certain criteria is met such as, but not limited to, a minimum BMI reading and participation in a comprehensive weight management program.
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- Benefits are subject to plan provisions including eligibility at the time services are rendered.
- Is the coverage full or is it at 50%?
- Varies by plan and state requirements
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Prior authorization may require certain criteria is met such as, but not limited to, a minimum BMI reading and participation in a comprehensive weight management program.
- Supporting Collateral:
- N/A.
- Covered Medications:
- Accounts contracted in California will not be able to collect medications intended for weight control.
Medications approved by the FDA for weight control, such as Zepbound, Wegovy, Saxenda, Victoza, and Exenatide, are not included in the California formulary. However, if a weight loss medication is being used to treat another medical condition, it may be covered if approved on appeal.
There may be confusion between medications like Tirzepatide (Mounjaro), which is a diabetes drug, and Zepbound, which is specifically for weight loss. The distinction lies in the dosing; one dose is for weight loss, while the other is for diabetes management. Some drugs that are prescribed for diabetes are also used for weight control due to their side effects.
Prior authorization reviews will be conducted by CVS Caremark-trained pharmacists, who will assess the diagnosis codes and treatment plans to determine whether the medication can be approved. Medical providers should submit a letter of medical necessity along with supporting clinical documentation, such as charts, notes, and test results.
If a member receives a prior authorization denial from CVS Caremark, they can appeal the decision to the insurance company. All CVS Caremark denial letters include instructions on how to appeal their adverse determination to Nippon Life Benefits.
- Accounts contracted in California will not be able to collect medications intended for weight control.
Sharp Health Plan
- Members need to consult with their PCP and have prior authorization submitted and reviewed for approval.
Currently, we do not have the updated details to share.
Sutter Health Plan
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Yes, if the drug is listed on the SHP Pharmacy Formulary.
The member must obtain prior authorization for the necessary treatment of morbid obesity.
Weight Loss Drugs are covered through Pharmacy benefits. Based on the Tier the medication falls under.
- Yes, if the drug is listed on the SHP Pharmacy Formulary.
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- The CVS Caremark PA Guideline requires the Patient to have a documented diagnosis of morbid obesity as defined by:
- A current body mass index (BMI) of greater than or equal to 40 kilograms per square meter OR
- A documented BMI of greater than or equal to 35 kilograms per square meter AND the patient has one or more comorbid conditions (cardiovascular disease, hypertension, dyslipidemia, diabetes, elevated waist circumference) OR other obesity-related medical condition (sleep apnea)
- And that all the following are met:
- There is documentation that the patient is actively enrolled in a weight loss program that involves a reduced calorie diet and increased physical activity adjunct to therapy
- The patient’s age is appropriate according to US Food and Drug Administration (FDA) labeling for the requested drug
- The patient is NOT receiving TWO drugs for weight loss at the same time
- The patient does NOT have any contraindications to the requested drug
- The requested drug is being used for an FDA-approved indication
- The CVS Caremark PA Guideline requires the Patient to have a documented diagnosis of morbid obesity as defined by:
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- No, it is based on medical necessity.
- Is the coverage full or is it at 50%?
- It depends on the Pharmacy benefits for the specific plan, and the Tier determined by the SHP Formulary.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Yes, documentation is required that the patient is actively enrolled in a weight loss program that involves a reduced-calorie diet and increased physical activity, adjunct to therapy.
- Beginning March 1, 2026, Sutter Health Plan will partner with Vida Health to provide members with personalized virtual health and wellness programs at no additional cost.
- Vida offers comprehensive support in areas such as weight loss, nutrition, fitness, stress management, and chronic condition care through an easy-to-use app featuring live coaching and clinical guidance.
- Members age 18 and older who wish to receive coverage for weight loss medications must enroll in a Vida weight loss program and demonstrate monthly engagement.
- Yes, documentation is required that the patient is actively enrolled in a weight loss program that involves a reduced-calorie diet and increased physical activity, adjunct to therapy.
- Supporting Collateral:
- Click here to view the general Pharmacy Benefits Flyer. The EOCs for each plan also have related information under Pharmacy Exclusions and Limitations.
- For more information or to enroll beginning March 1, 2026, members can visit vida.com/sutterhealthplan or contact Vida Member Support at 833-732-2242.
- Covered Medications:
- SHP Pharmacy Formulary: https://www.sutterhealthplan.org/pdf/sutter-health-plus/shp-formulary.pdf
- Dulaglutide: Brand name Trulicity. Listed on Page 51.
- Liraglutide: Brand names Victoza and Saxenda. Listed on page 16.
- Semaglutide: Brand names Ozempic, Wegovy, and Rybelsus. Listed on pages 51, 16, 51.
- Tirzepatide: Brand names Mounjaro and Zepbound. Listed on page 51, 16.
- SHP Pharmacy Formulary: https://www.sutterhealthplan.org/pdf/sutter-health-plus/shp-formulary.pdf
Total Benefit Solutions
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Weight Loss Drugs are not regularly covered by our plans for fully insured customers. Some exceptions can be made with our underwriting departments approval. However, our CVS Weight management program along with some other prior authorization bundles are available for self-insured customers who want to cover weight loss drugs.
- Our CVS Weight Management program provides support to members taking anti-obesity medications and includes expanded access to programs for proactive weight management. We have a three-pronged approach to coverage, cost and care that helps manage GLP-1 pharmacy expenses. We offer coverage that uses plan design and formulary options as the foundation and utilization management to bolster the care offered to members.
- With the rise of GLP-1 medications, both for anti-obesity and diabetes, a holistic approach to weight management can help you achieve your overall benefit goals. CVS Weight Management offers a solution to effectively manage GLP-1 medications. It first starts with benefits coverage. Today we see approximately two-thirds of self-funded plan sponsors include GLP-1s in their anti-obesity coverage. For those that cover anti-obesity, formulary management is essential to effective cost management. Through size, scale and negotiations with manufacturers, we drive lower net costs within the therapeutic class and lower plan and member costs.
- Our robust utilization management solutions ensure medications are used based on labeled indication and according to clinical guidelines. For anti-diabetic GLP-1s, we ensure clinically-appropriate use that limits member disruption. For anti-obesity products, we align to current clinical guidelines to ensure members meet body mass index (BMI) and weight loss thresholds to initiate and continue therapy.
- CVS Weight Management can be integrated with Aetna pharmacy benefits through a required co-therapy integration or voluntary participation. If you select the required co-therapy integration, members are required to enroll and participate in the program to have access to anti-obesity medication. You can also elect to make this program voluntary for members, allowing them access to the support they need without an impact on their drug coverage
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?
- To be eligible for the CVS Weight Management program, members must be:
- Age 18+
- MI ≥27 and an obesity-related comorbid condition
- BMI ≥30 + with/without comorbid condition.
* Obesity-related comorbid conditions include but are not limited to diabetes, prediabetes, hypertension, dyslipidemia, CAD, osteoarthritis and obstructive sleep apnea. Exclusion criteria apply.
- *OR Members currently taking an Anti-Obesity Medication (AOM) Members take a screening to determine their eligibility. Members may be excluded from the program based on certain clinical criteria
- To be eligible for the CVS Weight Management program, members must be:
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- Our CVS Weight Management program prescribes GLP-1 medications for weight loss under certain circumstances. As a best practice, we believe members should consult their primary care physician or other trusted provider to receive a prescription for weight loss medications.
- Is the coverage full or is it at 50%?
- Plan sponsor cover Weight Loss Drugs within their pharmacy plan.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Program options
- No Benefit Integration (Voluntary) – This is the Aetna International default recommendation.
- In a voluntary model, members are not required to engage in the program before or during weight management medication use, but for those that do receive the same program support
- Required Benefit Integration
- In a required model, members would have to engage in the program while on a weight management medication to maintain plan designated cost share for the medication and are offered the option to participate before use of the medication.
- No Benefit Integration (Voluntary) – This is the Aetna International default recommendation.
- Program options
- Supporting Collateral:
- Click here for more information on GLP-1 and the CVS Weight Management Program and use the below link:
- Covered Medications:
- Our CVS Weight Management program prescribes GLP-1 medications for weight loss under certain circumstances. As a best practice, we believe members should consult their primary care physician or other trusted provider to receive a prescription for weight loss medications.
UnitedHealthcare
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Covered for CA small business fully insured plans.
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?Are there coverage limits (e.g., 6 months, one year, etc.)?
- (BMI) of greater than or equal to 30 kg/m2 or 27 kg/m2 with an obesity-related comorbidity.
- Motivation-based wellness program participation and prior authorization are required before drug coverage.
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- No, limitations are noted currently, but Prior Authorization and Supply Limits apply.
- Is the coverage full or is it at 50%?
- GPL-1 covered medications in the PDL, cost-share applies based on Tier and the member’s Rx plan benefit.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Motivation-based wellness program participation and prior authorization are required before drug coverage.
- Supporting Collateral:
- N/A
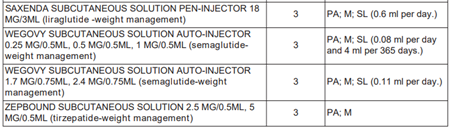
- Covered Medications:
- Please refer to the CA SB PDL lists for the GLP-1 medications covered. They all fall under Tier 3 of the member’s Rx plan benefit.
NOTED:- PA (prior authorization required)
- M (may be covered under the medical benefit with prior authorization for HMO plans
- SL (supply limits) as outlined in the PDL
- Please refer to the CA SB PDL lists for the GLP-1 medications covered. They all fall under Tier 3 of the member’s Rx plan benefit.
Western Health Advantage
- Do your plans cover Weight Loss Drugs (GLP-1) if deemed medically necessary? If so, how are they covered?
- Yes, when specific criteria are met.
- All weight loss products (oral and GLP1s) are not on formulary but can be accessed if approved through the prior authorization (PA) or non-formulary (NF) exceptions process.
- Are there any clinical criteria for approval (e.g., BMI level, sustained weight min/max, step therapy such as a weight loss management program)?Are there coverage limits (e.g., 6 months, one year, etc.)?
- Yes, there are criteria points, and they differ based on what drug (oral vs GLP1) is being requested.
For the most up-to-date clinical criteria, please visit the WHA website for PA and NF Criteria.
- Yes, there are criteria points, and they differ based on what drug (oral vs GLP1) is being requested.
- Are there coverage limits (e.g., 6 months, one year, etc.)?
- Yes, all approvals will be 6 months (initial and renewals) with ongoing coverage requiring updated chart notes that document all reauthorization criteria points as found on the WHA website (WHA PA and NF Criteria).
- Is the coverage full or is it at 50%?
- Weight loss drugs are not on formulary so when approved through the PA/NF process they will default to the highest applicable tier cost share.
- All diabetic GLP1s are on covered on tier 2 with a PA. Members should refer to this copayment summary for further details.
- Do members need to be enrolled in a comprehensive weight loss program before or concurrently receiving the weight loss drug?
- Members need to have tried and failed a reduced calorie diet and exercise of at least 150 minutes per week for at least 6 months prior to starting weight loss medication. The same lifestyle changes must be continued while on weight loss medication (documentation of such is required).
- Supporting Collateral:
- Formulary lookup tool can be used to see what drugs are and are not on formulary.
- Covered Medications:
- Dulaglutide: Brand name Trulicity
- FDA approved for Type 2 Diabetes Mellitus (T2DM) and requires a PA with chart notes documenting diagnosis (confirmed with lab values) and trial and failure with 30 days of metformin or another antidiabetic drug.
- Exenatide: Brand names Byetta and Bydureon
- Same as above.
- Liraglutide: Brand names Victoza and Saxenda
- Brand Victoza is non-preferred and requires same criteria as above + trial and failure with generic liraglutide and two preferred products (Ozempic, Rybelsus, Trulicity, Byetta, Bydureon, or Mounjaro). Saxenda is for weight loss and is held to the criteria mentioned in the third column.
- Lixisenatide: Brand Name Adlyxin
- This drug is no longer available in the United States. Soliqua (insulin glargine with lixisendatide) is available without a PA.
- Semaglutide: Brand names Ozempic, Wegovy, and Rybelsus
- Ozempic and Rybelsus are FDA approved for T2DM and are held to the same criteria as Trulicity. Wegovy is for weight loss and is held to the criteria mentioned in the third column.
- Tirzepatide: Brand names Mounjaro and Zepbound
- Mounjaro is only FDA approved for approved for T2DM and is held to the same criteria as Trulicity. Zepbound is for weight loss and is held to the criteria mentioned in the third column.
- Dulaglutide: Brand name Trulicity
Most Recent Articles
Industry News
Carrier Updates
Carrier Updates

